Background: BTK inhibitors and BCL2 antagonists as monotherapy are highly active and well tolerated in Waldenström macroglobulinemia (WM). We initiated a prospective study evaluating ibrutinib and venetoclax in treatment-naive WM. Study therapy was stopped on March 31, 2022, after four ventricular arrhythmia events, including two grade 5 events. Herein, we present follow-up data after stopping therapy to assess ongoing safety and response durability of this combination in WM.
Methods: This was an investigator-initiated, multicenter, prospective phase II study in symptomatic treatment-naïve WM patients. Study therapy was given in 4-week cycles. Intended therapy consisted of ibrutinib at 420 mg/day on cycle 1. Venetoclax was added on cycle 2 at 100 mg/day for one week, 200 mg/day for one week, and 400 mg/day for two weeks. Ibrutinib 420 mg/day and venetoclax 400 mg/day were given together for cycles 3-24. All patients underwent baseline laboratory studies, a bone marrow biopsy with MYD88 and CXCR4 genotyping, and CT scans to evaluate extramedullary disease. Responses were assessed using modified IWWM6 criteria. The study was registered under clinicaltrials.gov (NCT04273139).
Results: Between July 2020 and January 2022, 45 (30 males; 15 females) patients were enrolled. Baseline characteristics were: median age 67 (range 40-82 yrs); serum IgM 4297 (range 572-9211 mg/dL); hemoglobin 10.2 (range 7.8-15.3 g/dL); bone marrow involvement 60% (5-90%); presence of lymphadenopathy (>1.5 cm) 25 (56%); and splenomegaly (>15 cm) 13 (29%). MYD88 L265P was detected in all patients, and CXCR4 mutations in 17 (38%; 10 nonsense and 7 frameshift). Median time on treatment was 10.2 months (range 1.9-20.8) before treatment was halted. Overall response rate was 100%, and major response 96%. Best responses included very good partial response (VGPR; n=19, 42%); partial response (n=24, 53%); and minor response (n=2, 4%). CXCR4 mutations were associated with lower VGPR rates (29% v 50%; p=0.18).
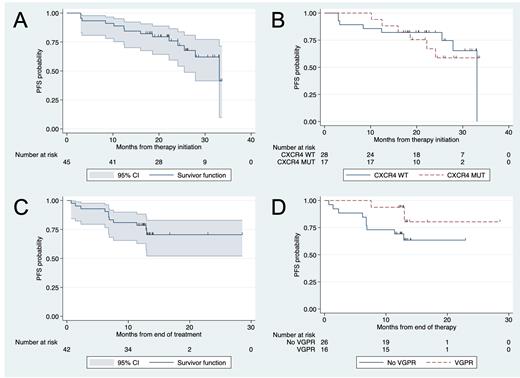
At a data cutoff date of May 31, 2023, the median study follow-up is 24.4 months (range 3-33.6). There were 12 progression events, including two treatment-emergent deaths and one transformation to DLBCL. Five patients started a new therapy. At 24 months, progression-free survival (PFS) rate was 76% (95% CI 59-86; Figure A), next treatment-free rate was 89% (95% CI 72-96), and overall survival (OS) rate was 96% (95% CI 84-99). CXCR4 mutations did not impact PFS (p=0.89; Figure B), time to next treatment (TTNT) (p=0.43), or OS (p=0.27). Median time after end of therapy (EOT) was 13.3 months (95% CI 12.9-13.5). There were 11 progression events after EOT, and the 12-month PFS rate after EOT was 79% (95% CI 63-88; Figure C). CXCR4 mutations (p=0.35) or time on therapy (<12 vs. ≥12 months; p=0.76) did not impact PFS after EOT. There was a trend towards longer PFS after EOT in patients who had attained VGPR (p=0.12; Figure D). No treatment-emergent events, especially arrhythmia, were observed after treatment stopped. Thirty-one patients underwent a bone marrow biopsy one year after EOT. No emergent mutations, especially in BTK and TP53, were detected.
Conclusion: In symptomatic, treatment-naive patients with WM, the combination of ibrutinib and venetoclax was shown to be highly effective with a VGPR rate of 42% and a 24-month PFS rate of 76%, despite stopping therapy early due to unexplained ventricular arrhythmia. VGPR attainment might predict longer PFS after EOT, and PFS was similar in patients who received <12 vs. ≥12 months of therapy. No treatment-emergent toxicities, including arrhythmia, occurred after EOT. The combination of ibrutinib and venetoclax holds significant promise. However, given that the cause of the unexpected ventricular arrhythmia remains unclear, it is challenging to recommend the combination at the current dose and schedule. The potential for shorter treatment durations or safer combinations offer hope for maintaining efficacy while mitigating adverse effects.
OffLabel Disclosure:
Castillo:Cellectar: Consultancy, Research Funding; BeiGene: Consultancy, Research Funding; Kite: Consultancy; Mustang Bio: Consultancy; Pharmacyclics: Consultancy, Research Funding; Abbvie: Consultancy, Research Funding; AstraZeneca: Consultancy, Research Funding; Loxo: Consultancy, Research Funding. Sarosiek:ADC Therapeutics: Research Funding; Cellectar: Consultancy, Research Funding; Beigene: Honoraria, Research Funding. Branagan:Genzyme: Membership on an entity's Board of Directors or advisory committees; CSL Behring: Membership on an entity's Board of Directors or advisory committees; BeiGene: Membership on an entity's Board of Directors or advisory committees; Karyopharm: Membership on an entity's Board of Directors or advisory committees; Sanofi: Membership on an entity's Board of Directors or advisory committees; Pharmacyclics: Membership on an entity's Board of Directors or advisory committees; Adaptive: Membership on an entity's Board of Directors or advisory committees. Treon:Eli Lilly: Consultancy, Research Funding; Bristoll Myers Squibb: Consultancy, Research Funding; BeiGene: Consultancy, Research Funding; Janssen: Consultancy, Research Funding; Abbvie/Pharmacyclics: Consultancy, Research Funding.
Venetoclax is not approved for the frontline treatment of Waldenström macroglobulinemia.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal